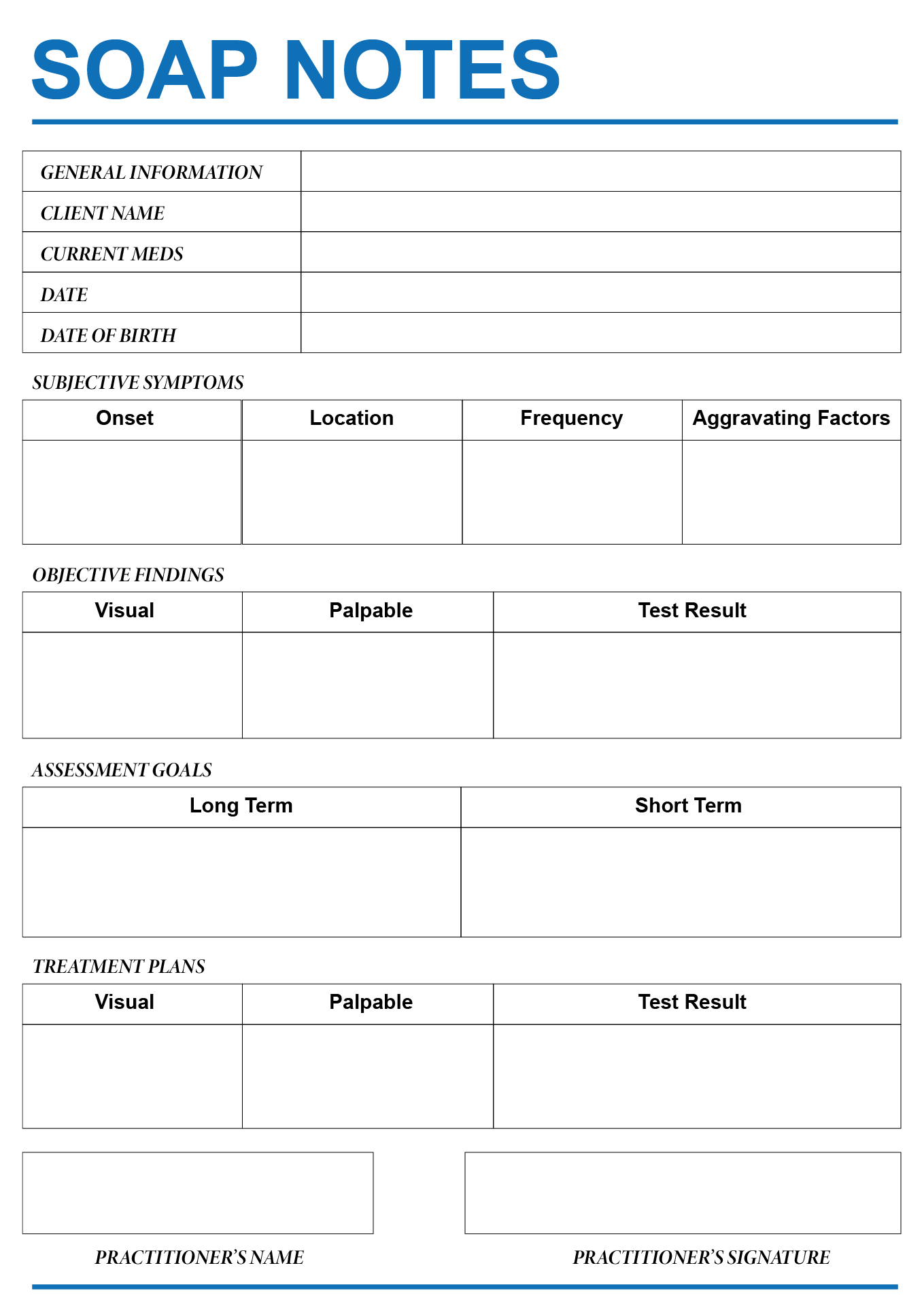
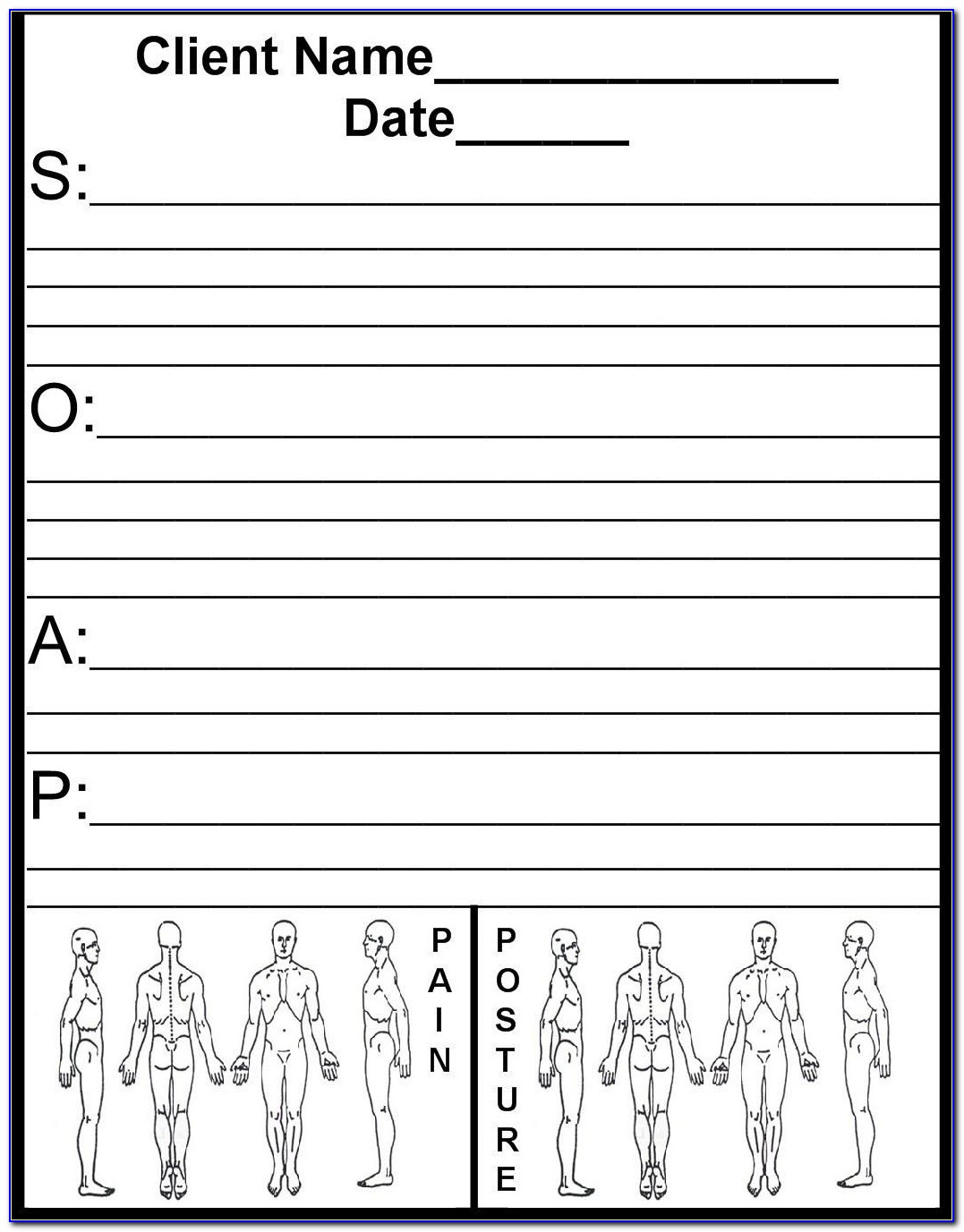
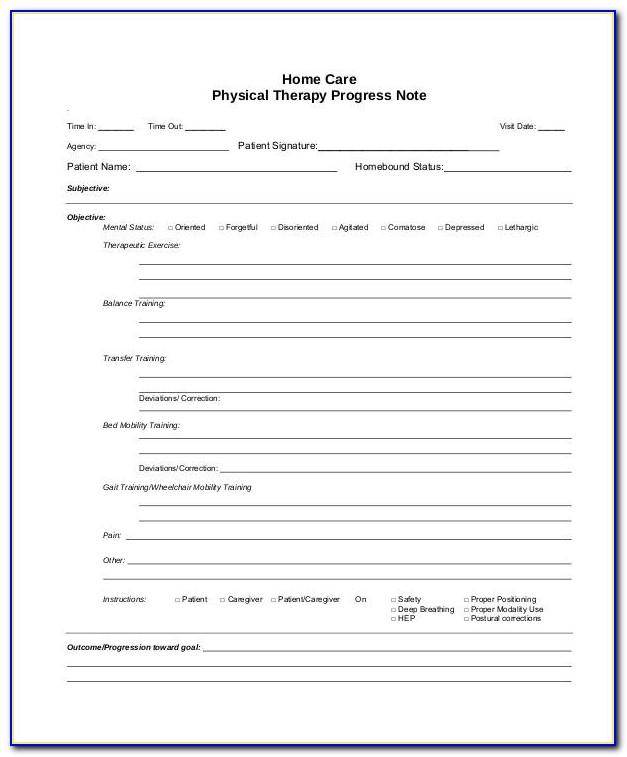
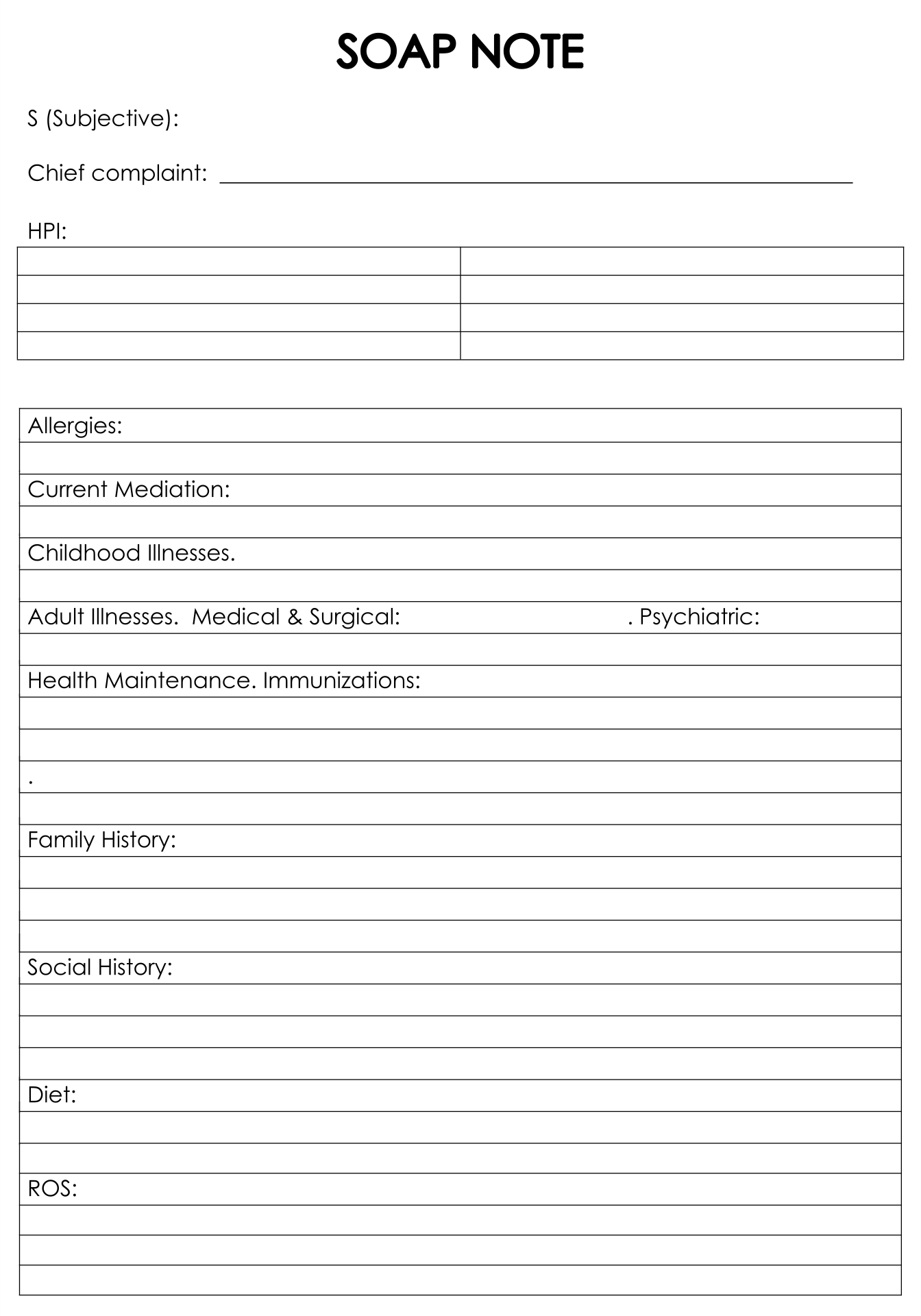
Soap Note Template Counseling - Counseling soap note in pdf; What makes a soap note effective? How to devise a detailed counseling soap note; All you have to do is access the pdf and fill in the relevant sections. Soap notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes. Using a template such as soap note means that you can capture, store and interpret your client's information consistently, over time. Where a client’s subjective experiences, feelings, or perspectives are recorded. Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Client was tearful during session with a sad affect and required pauses in. Subjective this covers your patient’s detailed medical history and current symptoms.
All you have to do is access the pdf and fill in the relevant sections. Web learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. For clinical professionals, soap notes offer a clear, concise picture of where the client is at the time of each session. Web the s.o.a.p acronym soap is an acronym for the 4 sections, or headings, that each progress note contains: Where a client’s subjective experiences, feelings, or perspectives are recorded. Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Here’s how to write soap notes. Web soap notes are easy to use and designed to communicate the most relevant information about the individual. Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Soap notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes.
Client was tearful during session with a sad affect and required pauses in. Here’s how to write soap notes. This might include subjective information from a patient’s guardian or someone else involved in their care. Web learn and become a pro in making professional soap note counselling templates with our stunning range of templates and examples. What makes a soap note effective? Web the s.o.a.p acronym soap is an acronym for the 4 sections, or headings, that each progress note contains: Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: What is a counseling soap note? Where a client’s subjective experiences, feelings, or perspectives are recorded. Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals.
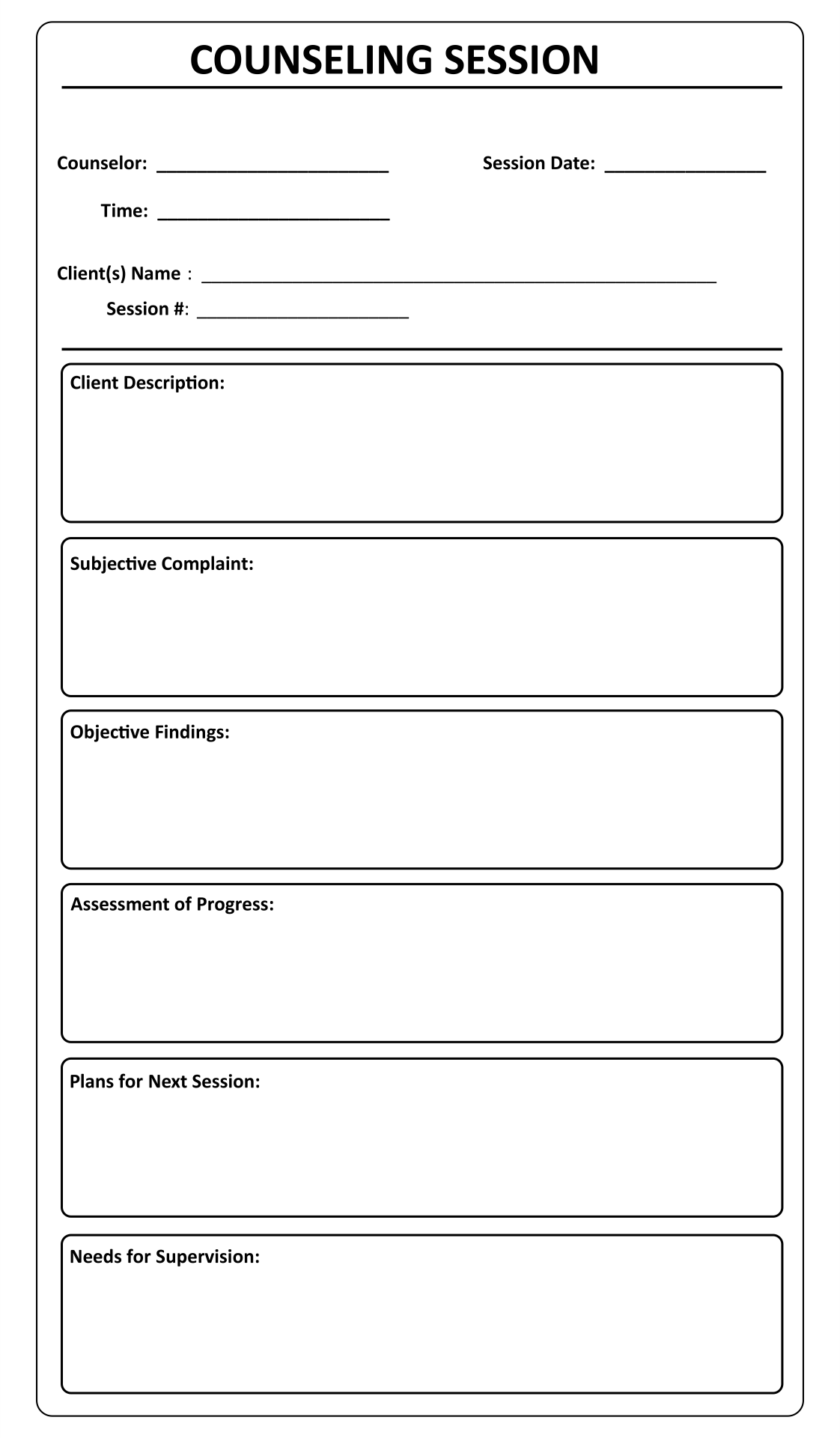
7 Best Images of Printable Counseling Soap Note Templates Counseling
Web learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Where a client’s subjective experiences, feelings, or perspectives are recorded. 3+ counseling soap note examples; This might include subjective information from a patient’s guardian or someone else involved in their care. Web objective identify your.
Soap Note Template Counseling
Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Client was tearful during session with a sad affect and required pauses in. Here’s how to write soap notes. Free to download and print. Web this soap note.
Free Counseling Soap Note Template Template Resume Examples o85pB0QqkZ
How to devise a detailed counseling soap note; This might include subjective information from a patient’s guardian or someone else involved in their care. Notes from your verbal interaction with patients as well as what they tell you about their condition go here. Web learning how to write a soap note can be one of the most effective ways for.
Image result for soap notes template for counseling Soap note
What makes a soap note effective? Where a client’s subjective experiences, feelings, or perspectives are recorded. Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. All you have to do is access the pdf and fill in the relevant sections. Web the s.o.a.p acronym soap is an.
Soap Note Template Counseling
Subjective this covers your patient’s detailed medical history and current symptoms. This might include subjective information from a patient’s guardian or someone else involved in their care. One of the best aspects of the soap note template is that the layout has already been organized for you. What is a counseling soap note? Web learn and become a pro in.
17 best Free Counseling Note Templates images on Pinterest Counseling
Our templates are useful for any type of health professionals. Web soap notes are easy to use and designed to communicate the most relevant information about the individual. For clinical professionals, soap notes offer a clear, concise picture of where the client is at the time of each session. One of the best aspects of the soap note template is.
Counseling Session Notes Template 7 Best Images of Printable
Subjective this covers your patient’s detailed medical history and current symptoms. Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. 3+ counseling soap note examples; All you have to do is access the pdf and fill in the relevant sections. What is a counseling soap note?
Psychiatry Soap Note Template
Where a client’s subjective experiences, feelings, or perspectives are recorded. Web learn and become a pro in making professional soap note counselling templates with our stunning range of templates and examples. What is a counseling soap note? Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Web in this post, we will review what soap.
7 Best Images of Printable Counseling Soap Note Templates Counseling
Web this soap note template is useful for counselors for a range of different reasons, including the following: What is a counseling soap note? Free to download and print. Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap.
10 Best Printable Counseling Soap Note Templates
This might include subjective information from a patient’s guardian or someone else involved in their care. Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Web objective identify your observations of the client in today’s session and.
For Clinical Professionals, Soap Notes Offer A Clear, Concise Picture Of Where The Client Is At The Time Of Each Session.
What is a counseling soap note? They can also provide documentation of progress. Using a template such as soap note means that you can capture, store and interpret your client's information consistently, over time. 3+ counseling soap note examples;
This Might Include Subjective Information From A Patient’s Guardian Or Someone Else Involved In Their Care.
Web learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Free to download and print. Subjective this covers your patient’s detailed medical history and current symptoms. All you have to do is access the pdf and fill in the relevant sections.
Web The S.o.a.p Acronym Soap Is An Acronym For The 4 Sections, Or Headings, That Each Progress Note Contains:
One of the best aspects of the soap note template is that the layout has already been organized for you. What makes a soap note effective? Notes from your verbal interaction with patients as well as what they tell you about their condition go here. Record your patient’s chief complaint, existing symptoms, and any pain description in this section.
How To Devise A Detailed Counseling Soap Note;
Web soap notes are easy to use and designed to communicate the most relevant information about the individual. Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Our templates are useful for any type of health professionals. Web this soap note template is useful for counselors for a range of different reasons, including the following: